Tendinitis (Tendinopathy)
What is Tendinitis?
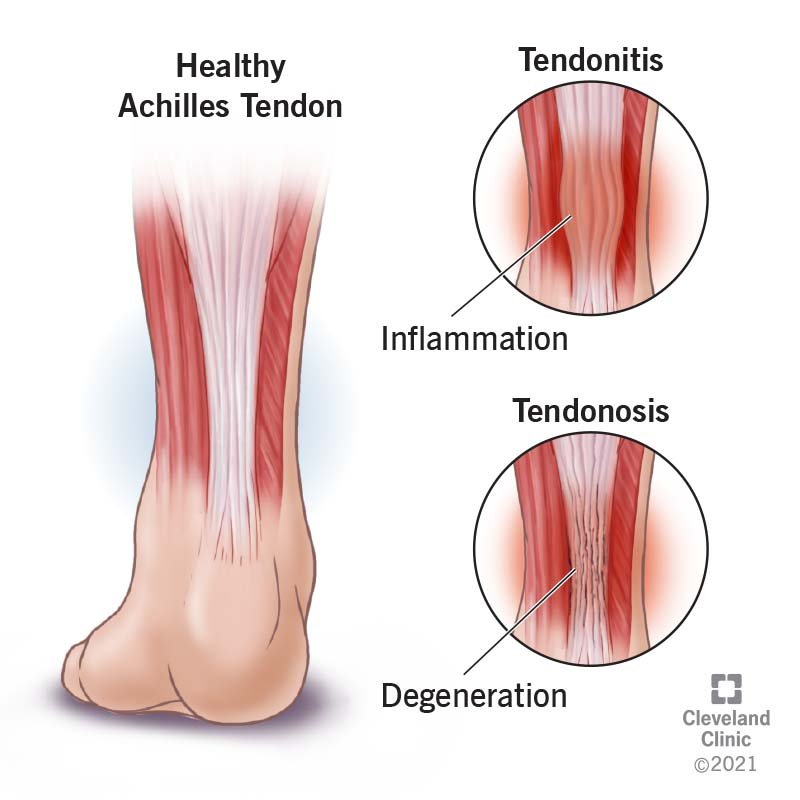
Tendinitis, also called tendinopathy (disease of tendon), refers to inflammation or degeneration (tendinosis) of a tendon—the thick, fibrous tissue connecting muscles to bones. It often results from repetitive strain, overuse, injury, or ageing.
General Symptoms of Tendinopathy
Pain and tenderness, particularly with activity
Stiffness and reduced movement in the affected area
Swelling or thickening of the tendon
Decrease function in the area due to pain and weakness
Common Areas Affected By Tendinopathy
Bicipital Tendinopathy (Shoulder)
Pain at the front of the shoulder, particularly with overhead activities or lifting
Often associated with repetitive lifting, throwing, or other overhead motions
Flexor and Extensor Tendinopathy (Elbow)
Pain either on the inner side (flexor tendinopathy, golfer’s elbow) or outer side (extensor tendinopathy, tennis elbow)
Typically caused by repetitive gripping, wrist movements, or elbow strain
Achilles Tendinopathy (Heel)
Pain at the back of the heel, especially noticeable during walking or running
Common in runners or individuals engaging in repetitive jumping or prolonged standing
Patellar Tendinopathy (Knee)
Pain just below the kneecap, often exacerbated by jumping, squatting, or stair climbing
Frequently occurs in athletes involved in sports with repetitive jumping or knee loading
Assessing Tendinopathies
Clinical assessment typically involves:
Thorough patient history to understand activity patterns and symptom development
Physical examination focusing on tenderness, swelling, and joint mobility
Imaging (such as ultrasound or MRI), if required, to confirm diagnosis and rule out other conditions
Typical Prognosis
With appropriate conservative treatment, most tendinopathies improve significantly over several weeks to months. Chronic or recurrent cases may require ongoing management and lifestyle modifications.
Evidence-Based Management
Clinical guidelines recommend:
Exercise Therapy: Specific strengthening and stretching exercises to improve tendon strength and flexibility.
Activity Modification: Adjusting or temporarily avoiding aggravating activities.
Manual Therapy: Techniques such as soft tissue mobilisation, joint mobilisations, and muscle release to improve function.
Pain Management: Short-term use of analgesics or anti-inflammatory medications, according to clinical guidelines.
Supportive Measures: Bracing, taping, or orthotic devices to support and reduce tendon strain.
Advanced Treatments: Shockwave therapy or injections for persistent cases, following clinical recommendations.